| |
Circumcision and HIV - the Randomised
Controlled Trials
'Circumcision Vindicated At Last!' ? - hardly
|
The American mind seems extremely vulnerable to the
belief that any alleged knowledge which can be
expressed in figures is in fact as final and exact as
the figures in which it is expressed.
- Richard Hofstadter, Anti-Intellectualism
in
American Life,
quoted by Charles Seife in Proofiness
|
After centuries of circumcision searching for a disease to
cure, and the emergence of a new one that is sexually
transmitted, it may be that a link has actually, finally
been found. This still falls very far short of justifying
Routine Infant Circumcision, however, despite the headline of a
Toronto columnist trumpetting "Circumcision Vindicated At Last!"
The latest
studies are the most careful so far to avoid the
mistakes of their predecessors:
|
National
Institute of Allergy and
Infectious Diseases (NIAID)
EMBARGOED FOR RELEASE
Wednesday, December 13, 2006
12:00 Noon ET
Adult Male Circumcision
Significantly Reduces Risk of Acquiring HIV
[A surgical miracle! No hint
of the many caveats to follow.]
Trials in Kenya and Uganda Stopped Early
The National Institute of Allergy and Infectious
Diseases (NIAID), part of the National Institutes of
Health (NIH), announced an early end to two clinical
trials of adult male circumcision because an interim
review of trial data revealed that medically performed
circumcision significantly reduces a man's risk of
acquiring HIV through heterosexual intercourse. The
trial in Kisumu, Kenya, of 2,784 HIV-negative men
showed a 53 percent reduction of HIV acquisition in
circumcised men relative to uncircumcised men, while a
trial of 4,996 HIV-negative men in Rakai, Uganda,
showed that HIV acquisition was reduced by 48 percent
in circumcised men. ["Impressive
sounding reductions in relative risk can mask much
smaller reductions in absolute risk." - editorial
in
the British Medical Journal, January 19,
2008. In fact they are inevitably greater, but
their actual utility depends on the absolute risk.]
"These findings are of great interest to public
health policy makers who are developing and
implementing comprehensive HIV prevention
programs,"says NIH Director Elias A. Zerhouni, M.D.
"Male circumcision performed safely in a medical
environment complements other HIV prevention
strategies and could lessen the burden of HIV/AIDS,
especially in countries in sub-Saharan Africa where,
according to the 2006 estimates from UNAIDS, 2.8
million new infections occurred in a single year."
"Many studies have suggested that male circumcision
plays a role in protecting against HIV acquisition,"
notes NIAID Director Anthony S. Fauci, M.D. "We now
have confirmation — from large, carefully controlled,
randomized clinical trials [the
randomisation was only in the assignment of the
paid volunteers to experimental or control groups;
they were not a random sample of the population.
The trials were not - by the nature of
circumcision, could not be - double blinded or
placebo controlled, the gold standard of clinical
trials.] — showing definitively that
medically performed circumcision can significantly
lower the risk of adult males contracting HIV through
heterosexual intercourse. While the initial benefit
will be fewer HIV infections in men, ultimately adult
male circumcision could lead to fewer infections in
women in those areas of the world where HIV is spread
primarily through heterosexual intercourse."
The findings from the African studies may have less
impact on the epidemic in the United States for
several reasons. In the United States, most men have
been circumcised. Also, there is a lower prevalence of
HIV. Moreover, most infections among men in the United
States are in men who have sex with men, for whom the
amount of benefit [if any]
provided by circumcision is unknown [but
is
likely to be much less, because HIV is known to be
more readily transmitted to the receptive male
partner]. Nonetheless, the overall
findings of the African studies are likely to be
broadly relevant regardless of geographic location: a
man at sexual risk who is uncircumcised is more likely
than a man who is circumcised to become infected with
HIV. Still, circumcision is only part of a broader HIV
prevention strategy that includes limiting the number
of sexual partners and using condoms during
intercourse. [In that case,
any benefit provided by circumcision would only
apply in the rare cases where a condom breaks or
comes off.]
The co-principal investigators of the Kenyan trial
are Robert Bailey, Ph.D., M.P.H., of the University of
Illinois at Chicago, and Stephen Moses, M.D., M.P.H.,
University of Manitoba, Canada. In addition to NIAID
support, the Kenyan trial was funded by the Canadian
Institutes of Health Research and included Kenyan
researchers Jeckoniah Ndinya-Achola, M.B.Ch.B., and
Kawango Agot, Ph.D., M.P.H. The Ugandan trial is led
by Ronald Gray, M.B.B.S., M.Sc., of Johns Hopkins
Bloomberg School of Public Health, Baltimore,
Maryland. Additional collaborators in the Ugandan
trial were David Serwadda, M.Med., M.Sc., M.P.H.,
Nelson Sewankambo, M.B.Ch.B., M.Med.M.Sc., Stephen
Watya, M.B.Ch.B., M.Med., and Godfrey Kigozi,
M.B.Ch.B., M.P.H.
Both trials involved adult, HIV-negative heterosexual
male volunteers assigned at random to either
intervention (circumcision performed by trained
medical professionals in a clinic setting) or no
intervention (no circumcision). All participants were
extensively counseled in HIV prevention and risk
reduction techniques.
[With AIDS running at 4.10%
in the population (according the the CIA's
World
Factbook), selecting men who are
HIV-negative means that already
- they are likely to have
some natural immunity
- they are likely to be
more careful than the average person and
the fact that they volunteer
implies they have more concern about HIV/AIDS than
others. These introduces biases that make
circumcision likely to be less effective when
applied to the general population.]
Both trials reached their enrollment targets by
September 2005 and were originally designed to
continue follow-up until mid-2007. However, at the
regularly scheduled meeting of the NIAID Data and
Safety Monitoring Board (DSMB) on December 12, 2006,
reviewers assessed the interim data and deemed
medically performed circumcision safe and effective in
reducing HIV acquisition in both trials. They
therefore recommended the two studies be halted early.
All men who were randomized into the non-intervention
arms will now be offered circumcision.
[For statistical reasons,
effectiveness of a treatment declines with the
passage of time. Cutting the experiment short
gives a falsely optimistic outcome.]
"It is critical to emphasize that these clinical
trials demonstrated that medical circumcision is safe
and effective when the procedure is performed by
medically trained professionals and when patients
receive appropriate care during the healing period
following surgery," notes Dr. Fauci.
[But once the meme
"Circumcision prevents HIV" is loose in the
community, this will be forgotten and
circumcisions will be done under unhygienic
conditions with shared instruments, quite possibly
under duress.]
Researchers have noted significant variations in HIV
prevalence that seemed, at least in certain African
and Asian countries, to be associated with levels of
male circumcision in the community. In areas where
circumcision is common, HIV prevalence tends to be
lower; conversely, areas of higher HIV prevalence
overlapped with regions where male circumcision is not
commonly practiced.
[These correlations require
highly selective use of statistics. There are many
exceptions: HIV is rare in Cuba, where
circumcision is also rare, and common in Lesotho,
where circumcision is common, and common among
both the Zulu of South Africa who do not
circumcise, and the Xhosa, who do.]
Results of the first randomized clinical trial
assessing the protective value of male circumcision
against HIV infection, conducted by a team of French
and South African researchers in South Africa, were
reported in 2005. That trial of more than 3,000
HIV-negative men showed that circumcision reduced the
risk of acquiring HIV by 60 percent. The trial was
funded by the French Agence Nationale de Recherches
sur le Sida (ANRS) (see http://www.anrs.fr/).
[Earlier studies claimed an
eight-fold reduction. As each new study corrects
the errors of its predecessors, the claimed
benefit goes down. In this, it resembles
parapsychological research. The suspicion arises
that when all confounding factors have been
allowed for, circumcision will confer no benefit
at all.
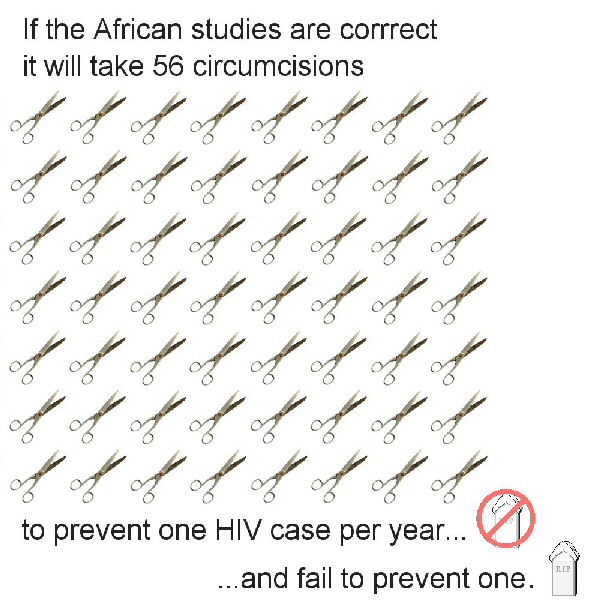
The Relative Risk Reduction
of 53% seems impressive, but when the rates of HIV
infection in the experimental and control
populations are considered, the results are less
impressive.
|
Cut infection rate in
12 months
|
1.58%
|
|
Intact infect. rate
in 12 months
|
3.38%
|
|
Absolute risk
reduction
|
1.8 (95% CI:
0.64-2.95)
|
|
Relative risk
reduction
|
53% (95% CI: 23-72)
|
|
Odds ratio
|
0.45 (95% CI:
0.27-0.77)
|
|
Number needed to
treat in 1 year
|
56 (95% CI:
34-155)
|
|
In other words, you
would have to circumcise 56 men to
prevent one of them contracting HIV in
one year.
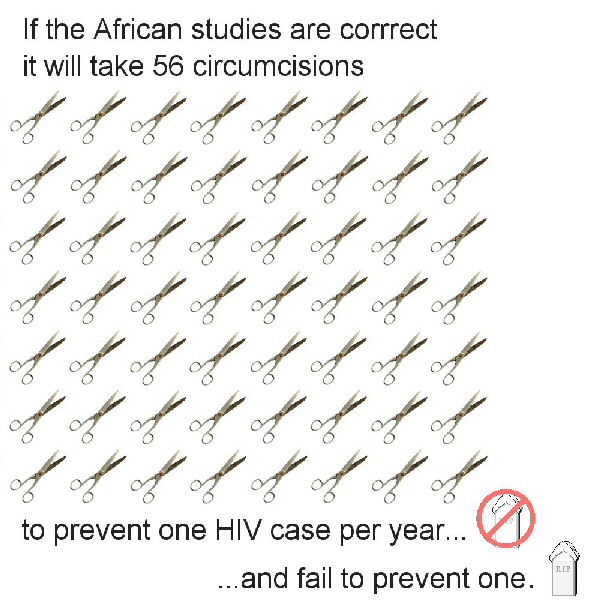 Click
on the image for an enlarged version
Click
on the image for an enlarged version
And the number needed
to prevent HIV longer term is higher.
Doctors could spend their time better
spent treating people with ulcerative
disease and malaria, which make HIV
transmission easier
and using the money saved to promote safer
sexual practices.
Few accepted medicines have such a high
NNT.
On this basis, the NNT in developed
countries such as the USA, where the HIV
rate is relatively low (0.6% compared to
4.1% in Uganda), would be much higher - it
would take 380 circumcisions in
the US to prevent one case of HIV.
|
For more information on the Kenyan and Ugandan trials
of adult male circumcision, see the NIAID Questions
and Answers document at http://www3.niaid.nih.gov/news/QA/AMC12_QA.htm.
|
...
4. What is adult male circumcision and
how was it performed in these studies?
... The circumcision procedure used in the
Kenyan trial was the foreskin clamp method.
... [This is
substantially the same as the tribal
method, blamed in Lesotho, where AIDS is
rife, for not taking enough mucosa]
The Kenyan trial procedure took about 25
minutes and used stitches to control
bleeding and improve wound closure. The
circumcision procedure used in the Ugandan
trial is known as the sleeve method and
takes about 30 minutes. [This
can take a variable amount of mucosa
depending where the "sleeve" is taken
from] The Ugandan trial used
cauterization of the blood vessels to
control bleeding and stitches to close the
wound. Both methods are commonly used
throughout the world.
.... Both trials recruited healthy,
HIV-negative uncircumcised men who planned
to remain near the study site for the
duration of the trial.
[This selects for
any natural immunity, and weeds out
itinerants, such as truck-drivers, who
are at higher risk of HIV, because of
their greater variety of partners.]
...men in the trials were cautioned to not
resume sexual activity until the incision
was fully healed and checked by the
physician....
|
From the Manual
of
Male Circumcision (October
2006), p 62
Avoid any sport, strenuous
activity, masturbation or sexual
intercourse for four to six weeks.
The healing process is well
advanced by 7 days but it takes 3
to 4 weeks for the wound to become
fully strong. Sexual intercourse
can be started after 4 to 6 weeks,
but it is best to use a condom as
this helps protect the newly
healed wound. It is always wise to
use a condom if there is any risk
of HIV infection. This is
particularly important after
circumcision as the newly healed
wound may be a weak point for two
or three months.
|
[As with the
Orange Farm study, this makes a
significant difference between the
experimental (cut) and control (intact)
group. The control group could have been
given a placebo operation, or another
kind of placebo, and the same
instructions. Even then, since the test
can not be made double blind (neither
experimenters nor subjects knowing who
is circumcised), errors will occur.]
...As with most prevention strategies,
adult male circumcision is not completely
effective at preventing HIV transmission. Millions of circumcised
men have become infected with HIV
through heterosexual exposure to the
virus. Men who receive adult
male circumcision may perceive that they are
at decreased risk for transmission and,
therefore, may not maintain other risk
reduction strategies. Modest increases in
the number of sexual partners could negate
the protective effect and increase the rate
of HIV transmission in a community. Adult
male circumcision will be most effective
when integrated into a comprehensive
prevention strategy which includes the ABCs
(Abstinence, Be Faithful, and Condoms) of
HIV prevention.
[This is the Nail Soup method
of using circumcision to prevent HIV.]
The World Health Organization (WHO) press
statement in response to the NIAID DSMB
recommendation is available on the WHO web
site, www.who.int/hiv.
|
And from http://www.who.int/mediacentre/news/notes/2006/np18/en/
WHO, UNFPA, UNICEF
and the UNAIDS Secretariat
emphasize that their current
policy position has not
changed and that they do not
currently recommend the
promotion of male circumcision
for HIV prevention purposes.
However, the UN recognizes the
importance of anticipating and
preparing for possible
increased demand for
circumcision if the current
trials confirm the protective
effect of the practice.
|
To a summary
critique of HIV claims.
|
|
An earlier
study:
|
Abstract
Impact of male circumcision on the female-to-male
transmission of HIV Auvert B.1, Puren A.2,
Taljaard D.3, Lagarde E.4, Sitta
R.4, Tambekou J.4
1 UVSQ - INSERM U687 - APHP, ST
Maurice CEDEX, France, 2 NICD, Johannesburg, South
Africa, 3 Progressus CC, Johannesburg, South Africa,
4 INSERM U687, St Maurice, France
Introduction: Observational studies suggest
that male circumcision could protect against HIV-1
acquisition. A randomized control intervention trial
to test this hypothesis was performed in sub-Saharan
Africa with a high prevalence of HIV and where the
mode of transmission is through sexual contact.
Methods: 3273 uncircumcised men, aged 18-24
and wishing to be circumcised,
were randomized in a control and intervention group.
Men were followed for 21 months with an inclusion
visit and follow-up visits at month 3, 12 and 21. Male
circumcision was offered to the intervention group
just after randomization and to the control group at
the end of 21 month follow-up visit. Male
circumcisions were performed by medical doctors. At
each visit, sexual behavior was assessed by a
questionnaire and a blood sample was taken for HIV
serology. These grouped censored data were analyzed in
an “intention to prevent” univariate and multivariate
analysis using the piecewise survival model, and
relative risk (RR) of HIV infection with 95%
confidence interval (95% CI) was determined.
Results: Loss to follow-up was <11%; <1%
of the intervention group were not circumcised and
< 2% of the control group were circumcised during
the follow-up. We observed 45 HIV infections in the
control group and 15 in the intervention group,
RR=2.77 (95% CI: 1.56 – 4.91; p=0.0005). When
controlling for sexual behavior, including condom use
and health seeking behavior, the RR was unchanged:
RR=2.93 (p=0.0003).
Conclusions: Male circumcision provides a high
degree of protection against HIV infection
acquisition. Male circumcision is equivalent
to
a vaccine with a 63% efficacy. The promotion of
male circumcision in uncircumcised males will reduce
HIV incidence among men and indirectly will protect
females and children from HIV infection. Male
circumcision must be recognized as an important means
to fight the spread of HIV infection and the
international community must mobilize to promote it.
|
|
Some
factors casting doubt on the findings:
-
A summary
of the study includes this:
|
Inclusion criteria:
...
Consenting to avoid sexual contact
(except with condom protection) during
the 6 weeks following the medicalized
circumcision
|
The
experimental (circumcised) men, but not the
control group (left intact), were
told:
|
When you are circumcised you will be
asked to have no sexual contact in the 6
weeks after surgery. To have sexual
contact before your skin of your penis
is completely healed, could lead to
infection if your partner is infected
with a sexually transmitted disease. It
could also be painful and lead to
bleeding. If you desire to have sexual
contact in the 6 weeks after surgery,
despite our recommendation, it is
absolutely essential that your (sic)
use a condom.
|
So:
1.
The circumcised experimental group, but not the
intact control group, got into the HABIT of
using condoms
2. They learnt HOW to use condoms
3. They had to make sure they HAD condoms (which
are in scandalously short supply in South
Africa), and
4. last but not least, they were PROTECTED by
condoms.
The
researchers could hardly say to the experimental
group, "but after that you don't have to use
condoms" could they?
Meanwhile
the intact control group was not required to use
condoms for the first six weeks of the study,
just sent out to take their chances.
This
throws the results into, er, a cocked hat.
- The
circumcised men would have had to take some time
away from any sexual activity, reducing their
exposure to HIV.
- The
circumcised men would inevitably get more exposure
to safe-sex information during their time in
medical hands, waiting for and recovering from,
their operations.
- Humans
are not lab rats. They have sex in non-random
ways. Many of the men in the study would put
themselves at little or no risk of contracting
HIV, a few at great risk, so the effective sample
size is much smaller than it appears, making the
margin of error much larger.
- Because
HIV-positive men were excluded from the study,
there would have been a higher proportion of men
with natural immunity in both groups than the
general population, reducing the effective sample
size still further.
- Because
all the subjects did not just agree to be
circumcised but wished to be, they were
not a representative sample of the general
population.
- 11-14
percent of the original participants (360 - 458
men) were lost to study or disqualified from
continuing. Their HIV status and/or circumcision
status might not be typical of the total (for
example, if they dropped out because they lost
interest in the experiment when they found
circumcision had not protected them), introducing
sufficient bias to refute the claimed finding.
- Michel
Garenne of the Institut Pasteur in Paris points
out that the
claimed
63% efficacy is not comparable to that of a
vaccine and would result in considerable
infection over time.
- Jennifer
Vines, MD, of the Oregon Health & Science
University in Portland, comments
"...the authors did not control for other sources
of HIV transimission such as blood transfusions or
exposure through infected needles. ... Controlling
for this route of infection could result in a
smaller difference between HIV infection rates in
the circumcised versus uncircumcised groups,
indicating that circumcision may not be as
effective at decreasing HIV transmission as the
article suggests."
- Columnist
Stephen Strauss (below)
points out that the study was cut short before
even half as many men were infected as were
infected before it began.
- The
Lancet (which earlier published a strident
call for circumcision by Robert Bailey) refused to
publish the study (apparently with ethical
concerns about not telling men they had HIV). The
study has been published by the Public
Library
of Science, an "open source" online medium.
- The
Abstract of the AIDS Conference in Rio reported 15
seroconversions from the circumcised group and 45
seroconversions in the uncircumcised group. (The
New Scientist, 6 August, reported 15
seroconversions in the circumcised group but 51 in
the uncircumcised group. On 29 July the Science
and Development Network reported 18
seroconversions in the circumcised group and 51 in
the uncircumcised group.) On 23 October, PLoS
reported that there were 20 seroconversions in the
circumcised group and 49 in the uncircumcised
group. From the official figures: 15-45 at the
AIDS Conference in Brazil and 20-49 in the PLoS
Journal, between 1 August and 23 October there
appear to have been 4 seroconversions among the
uncircumcised and 5 seroconversions among the
circumcised: in less than 3 months, a 3:1
difference has shrunk to 2.45:1 difference.
- We've
seen it many times before. Circumcision is touted
as the great panacea for this or that dreaded
disease of the age - but as the studies are
refined, the advantage withers away.
- The
rampant evangelism of the Conclusion suggests that
the experimenters are not altogether detached.
Even
if the findings are correct:
- If
they are acted on outside this controlled setting,
men with a keratinised,
reduced penis would be less likely to use condoms.
- The
biggest danger, still unmeasured, is that the
mantra "Circumcision prevents AIDS" will become
widespread, and circumcised men will take no other
precautions, spreading more HIV than their
circumcision prevents. Beliefs like "Sex with a
virgin cures AIDS" are already widespread in
Africa. Circumcision is a painful, memorable
operation that makes a permanent, visible change
to the penis: it would be a resolute man who
didn't feel it had made him safer - and therefore
act less safely.
-
There is some suggestion that circumcision
increases male-to-female
transmission. If so, promoting it could be
disastrous.
- As
UNAIDS said in
2000, relying on circumcision to protect against
AIDS if it offers only this level of protection is
like playing Russian roulette (with one bullet in
the chamber instead of three).
Relying on circumcision to halt the AIDS epidemic
is like fighting a housefire with a soda-syphon.
- While
a vaccine can be improved, this quite limited
preventive effect is as much as circumcision can
ever possibly give.
- Rather
than "Circumcision prevents HIV transmission" it
would put matters in a better perspective to say
"Circumcision (on average) delays HIV
transmission". If the findings of this study are
correct, where an intact man can expect to be
infected with HIV after a year, for a circumcised
man it would take two years more.
- "Protective
effect" over time depends not only on the
reduction in transmission per year, but also the
incidence (baseline rate of transmission).
Where
incidence is high, as it is in Africa,
"protective effect" over time is much less than
the figure for one year would suggest.
- So
rather than say "therefore men should be
circumcised (to make unprotected sex somewhat
safer)", the message should be "intact men should
be especially sure that the sex they have is
protected."
- In
STATS, Rebecca
Goldin points out that the low HIV/AIDS rate in
the US means it would require 10,000 circumcisions
to prevent 5.5 HIV infections, so the risks of
circumcision are at least comparable.
- This
(perhaps) makes a case for voluntary adult
circumcision. Babies still have a right not to be
second-guessed about their sexual practice 16 or
so years from now, the availability of a vaccine
then, or their wishes about what parts of their
body they may keep.
|
|
The misleading Relative Risk Ratio
Newspapers like big numbers and eye-catching
headlines. They need miracle cures and hidden scares,
and small percentage shifts in risk will never be
enough for them to sell readers to advertisers
(because that is the business model). To this end they
pick the single most melodramatic and misleading way
of describing any statistical increase in risk, which
is called the 'relative risk increase'. [Or
"Reduction" in the case of circumcision and HIV]
Let's say the risk of having a heart attack in your
fifties is 50 per cent higher if you have high
cholesterol. That sounds pretty bad. Let's say the
extra risk of having a heart attack if you have high
cholesterol is only 2 per cent. That sounds OK to me.
But they're the same (hypothetical) figures. Let's try
this. Out of a hundred men in their fifties with
normal cholesterol, four will be expected to have a
heart attack; whereas out of a hundred men with high
cholesterol, six will be expected to have a heart
attack. That's two extra heart attacks per hundred.
Those are called 'natural frequencies'.
Natural frequencies are readily understandable,
because instead of using probabilities, or
percentages, or anything even slightly technical or
difficult, they use concrete numbers, just like the
ones you use every day to check if you've lost a kid
on a coach trip, or got the right change in a shop.
Lots of people have argued that we evolved to reason
and do maths with concrete numbers like these, and not
with probabilities, so we find them more intuitive.
Simple numbers are simple.
The other methods of describing the increase have
names too. From our example above, with high
cholesterol, you could have a 50 per cent increase in
risk (the 'relative risk increase'); or a 2 per cent
increase in risk (the 'absolute risk increase'); or,
let me ram it home, the easy one, the informative one,
an extra two heart attacks for every hundred men, the
natural frequency.
As well as being the most comprehensible option,
natural frequencies also contain more information than
the journalists' 'relative risk increase'.
"Bad Science" by Ben Goldacre, Fourth
Estate, London (2008), p 256-9
[So here are the natural
frequencies:
The much-quoted "60% reduction" in HIV transmission
after circumcision amounts to about 12
non-circumcised men per thousand infected per year,
and about 6 circumcised men per thousand per year in
those countries the trials were held in, where HIV
is rampant - far fewer where it is rarer, such as
the US.]
|
|
"... [P]hysicians have a moral
obligation to handle medical statistics in ways that
minimize unconscious bias. Otherwise, they cannot
help but inavertently manipulate both their patients
and one another ...
Sam Harris, "The Moral Landscape"
Random House 2010, p 143
|
The three trials compared
So far as we know, the results of the three trials are nowhere
else presented side by side. Their figures are not always
presented in comparable formats.
| Study |
Orange Farm, S A |
Kisumu, Kenya |
Rakai, Uganda |
Total |
| Author |
Auvert |
Bailey, Moses |
Gray, Quinn, Wawer |
|
| Publication |
PLOS Medicine |
The Lancet |
The Lancet |
|
| Date |
November 2005 |
February 24, 2007 |
February 24, 2007 |
|
| Number recruited |
3,274 |
2,784 |
4,996 |
11,054 |
|
| Method |
forceps-guided |
forceps-guided |
sleeve
procedure |
|
| |
Control (intact) |
Exper (cut) |
Control (intact) |
Exper (cut) |
Control (intact) |
Exper (cut) |
Control (intact) |
Exper (cut) |
|
| HIV- at start |
1,582 |
1,546 |
1,393 |
1,391 |
2,522 |
2,474 |
5,497 |
5,411 |
10,908 |
Total lost from study
(corrected
Mar
24, 2008) |
151 |
100 |
92 |
87 |
133 |
140 |
376 |
327 |
703 |
| Proportion lost from study |
9.5% |
6.5% |
9.6% |
10.1% |
5.3% |
5.7% |
6.8% |
6.0% |
6.4% |
| HIV+ |
45 |
20 |
47 |
22 |
45 |
22 |
137 |
64 |
201 |
| HIV+ (%) |
2.84% |
1.29% |
3.37% |
1.58% |
1.78% |
0.89% |
2.49% |
1.18% |
1.8% |
Absolute risk
reduction (%) |
|
1.55% |
|
1.79% |
|
0.90% |
|
1.31% |
|
| number “protected” |
|
25 |
|
25 |
|
23 |
|
73 |
|
“Protection” - raw
(Relative Risk Reduction) |
|
60% (95% CI: 32%-76%) |
|
53% (22-72) |
|
55% (95% CI 22-75; p=0·002) |
|
| - controlled |
|
61% (95% CI: 34%-77%) |
|
60% (32-77) |
|
60% (30-77; p=0·003) |
|
| Number to treat |
|
34 |
|
30 |
|
55 |
|
39 |
|
Method:
|
The foreceps-guided method, in which the foreskin is
pulled forward and cut, removes significantly less
mucosa than the sleeve procedure in which a strip of
tissue is taken from behind the glans (and a method
like the forceps-guided has been blamed for the high
rate of HIV infection in Lesotho, where most men are
circumcised). Yet the degree of HIV reduction is
substantially the same for the two methods -
suggesting circumcision is not what is causing the
difference.
|
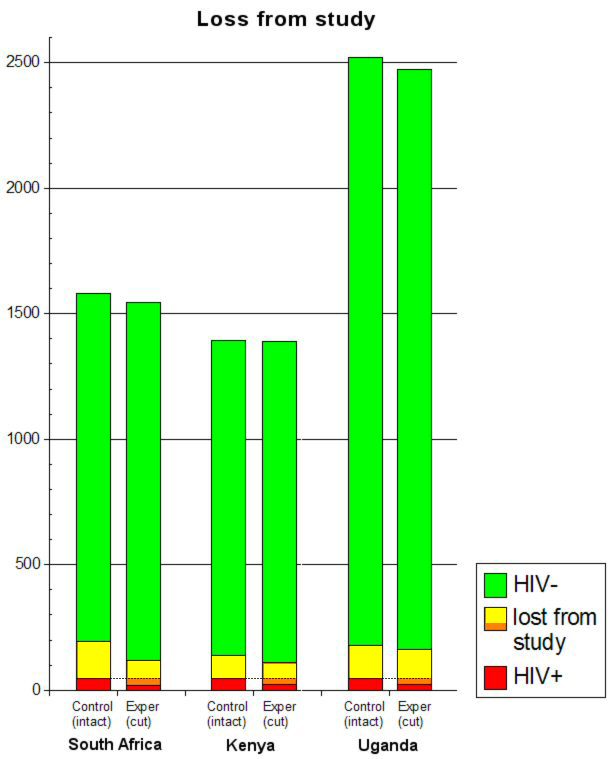
Loss from study
|
Ignore droputs
People who drop out of trials are statistically much
more likely to have done badly, and much more likely
to have had side-effects. They will only make your
drug look bad. So ignore them, make no attempt to
chase them up, do not include them in your analysis.
"Bad Science" by Ben Goldacre, Fourth
Estate, London (2008), p 209
|
|
All three trials had significant numbers "lost from
study", their HIV status unknown
(yellow+orange bars in the graphs below) - 100
circumcised subjects (6.5%) in South Africa, 87 (10%)
in Kenya and 140 (3.5%) in Uganda. (The figures are
presented confusingly in the studies because the men
did not all enter the trials together, but each trial
was stopped at a stroke.)
Those figures are high enough in themselves to cast
doubt on the validity of the results, but circumcised
men who found they had HIV would be disillusioned with
the trials and less likely to return. It would take
only 25, 25 and 23 such men respectively to completely
nullify the trials, and fewer to render the results
non-significant.
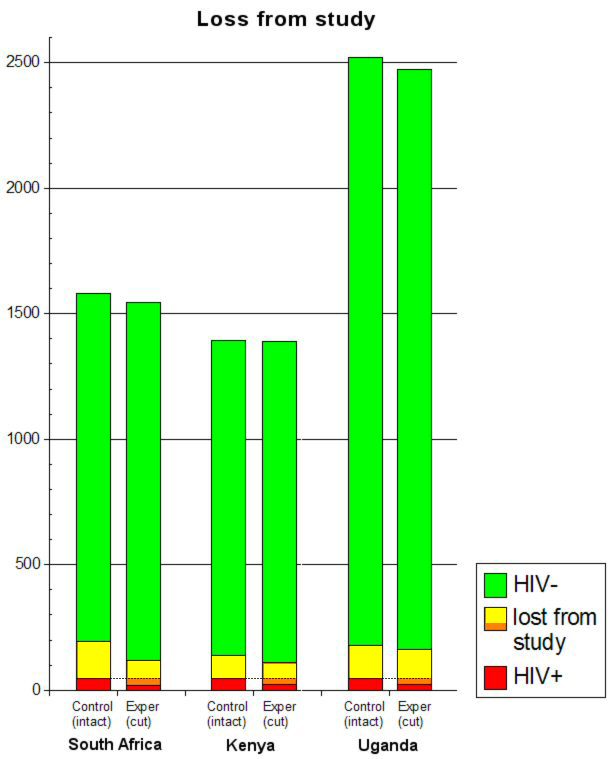
The orange part of each of the three right-hand bars
(below the dotted lines) represents the much-hyped
"60% protection" conferred by circumcision. If just
those men, whose HIV status is unknown, proved in fact
to be HIV+ (red), circumcision would certainly
have no protective effect whatever, but it would
not take all of them to reduce the effect below
statistical significance.
(One objection to this argument is that approximately
equal numbers of non-circumcised control-group members
dropped out. The answer to that is that a major and
very likely motivation for them to drop out would be
completely different and inapplicable to the
experimental group - to avoid getting circumcised.
Thus what needs explaining is why nearly equal numbers
of circumcised men dropped out, and an HIV+ diagnosis
could be an answer in a significant number of cases.)
|
Non-sexual transmission
|
In the South African trial, one third (23 of 69) of
the HIV infections occurred in men who reported no
unprotected sex during the period from their
last negative test to their first positive test. In
Uganda, 16 of 67 new infections occurred in men who
reported no sex partners (6 infections) or
100% condom use (10 infections). The trial in Kenya
did not report how sexual exposures related to HIV
incidence, except for seven men infected in the first
three months (sensitive tests did not find HIV in the
men's blood at the beginning of the trial). Five of
those seven, including three of four who had been
circumcised, reported no sexual exposures from
the beginning of the trial until their first
HIV-positive test.
|
Blood-borne transmission
|
The studies ignored exposure to HIV by blood.
In the two studies that reported information on
genital symptoms, 30-43% of infections with HIV
occurred during intervals when men reported genital
ulcers or other genital symptoms or problems. Because
genital symptoms were more common in uncircumcised
men, they may have been more likely to contract HIV
from skin-piercing procedures such as injections to
treat genital symptoms, but the studies did not
consider that possibility. None of the studies
reported on injections or on any other blood exposures
during follow-up. In the Kenyan trial, four men became
HIV-positive a month after circumcision, so the
circumcision itself might have infected them, but the
study did not mention that possibility.
|
Effect of cutting the studies short
|
'The best of five ... no ... seven ... no ...
nine!"
If the difference between your drug and placebo
becomes significant four and a half months into a six
month trial, stop the trial immediately and start
writing up the results: things might get less
impressive if you carry on.. Alternatively, if at six
months the results are 'nearly significant', extend
the trial by another three months.
"Bad Science" by Ben Goldacre, Fourth
Estate, London (2008), p 210
|
|
Randomized trails stopped early for benefit: a
systematic review.
Montori VM, Devereux PJ, Adhikari NK, et al.
JAMA 2005; 294:2203-09
Conclusion
Randomized clinical trials stopped early for benefit
are becoming increasingly common, particularly in top
medical journals. Adequate descriptions of the methods
used to inform the decision to truncate the trial are
often lacking. Trials stopped
early for benefit, particularly those with few
events, often report treatment effects that are
larger than typical of interventions that have been
definitively studied. These considerations
suggest that clinicians should view
results of RCTs stopped early for benefit with
skepticism.
|
|
Stopping Randomized Trials Early for Benefit and
Estimation of Treatment Effects
Systematic Review and Meta-regression Analysis
D. Bassler, M. Briel, V. M. Montori, M. Lane, P.
Glasziou, Qi Zhou, D. Heels-Ansdell, S. D. Walter, G.
H. Guyatt and the STOPIT-2 Study Group
JAMA. 2010;303(12):1180-1187
ALTHOUGH RANDOMIZED CONtrolled trials (RCTs)
generally provide credible evidence of treatment
effects, multiple problems may emerge when
investigators terminate a trial earlier than planned,
especially when the decision to terminate the trial is
based on the finding of an apparently beneficial
treatment effect. Bias may arise because large random
fluctuations of the estimated treatment effect can
occur, particularly early in the progress of a trial.
When investigators stop a trial based on an apparently
beneficial treatment effect, their results may
therefore provide misleading estimates of the benefit.
Statistical modeling suggests that RCTs stopped early
for benefit (truncated RCTs) will systematically
overestimate treatment effects, and empirical data
demonstrate that truncated RCTs
often show implausibly large treatment effects.
...
Context
Theory and simulation suggest that randomized
controlled trials (RCTs) stopped early for benefit
(truncated RCTs) systematically overestimate treatment
effects for the outcome that precipitated early
stopping.
Objective
To compare the treatment effect from truncated RCTs
with that from metaanalyses of RCTs addressing the
same question but not stopped early (nontruncated
RCTs) and to explore factors associated with
overestimates of effect.
Data Sources
Search of MEDLINE, EMBASE, Current Contents, and
full-text journal content databases to identify
truncatedRCTs up to January2007; search ofMEDLINE,
Cochrane Database of Systematic Reviews, and Database
of Abstracts of Reviews of Effects to identify
systematic reviews from which individual RCTs were
extracted up to January 2008.
Study Selection
Selected studies were RCTs reported as having stopped
early for benefit and matching nontruncated RCTs from
systematic reviews. Independent reviewers with medical
content expertise, working blinded to trial results,
judged the eligibility of the nontruncated RCTs based
on their similarity to the truncated RCTs.
Data Extraction
Reviewers with methodological expertise conducted data
extraction independently.
Results
The analysis included 91 truncated RCTs asking 63
different questions and 424 matching nontruncated
RCTs. The pooled ratio of relative risks in truncated
RCTs vs matching nontruncated RCTs was 0.71 (95%
confidence interval, 0.65-0.77). This difference was
independent of the presence of a statistical stopping
rule and the methodological quality of the studies as
assessed by allocation concealment and blinding. Large
differences in treatment effect size between truncated
and nontruncated RCTs (ratio of relative risks
<0.75) occurred with truncated RCTs having fewer
than
500 events. [The
three HIV-circumcision RCTs had a total of 196
events] In 39 of the 63 questions
(62%), the pooled effects of the nontruncated RCTs
failed to demonstrate significant benefit.
|
Comment
...On average, the ratio of RRs in the
truncated RCTs and matching nontruncated
RCTs was 0.71. This implies that, for
instance, if the RR from the nontruncated
RCTs was 0.8 (a 20% relative risk
reduction), the RR from the truncated RCTs
would be on average approximately 0.57 (a
43% relative risk reduction, more than
double the estimate of benefit).
Nontruncated RCTs with no evidence of
benefit—ie, with an RR of 1.0— would on
average be associated with a 29% relative
risk reduction in truncated RCTs addressing
the same question.
[This suggests
that the three HIV-circumcision RCTs
would have showed much less benefit -
none? - if they had not been truncated.
Circumcision advocates mention the
curtailing of the trials as an
indication of how beneficial
circumcision is, when the reverse may be
the case.]
|
Conclusions Truncated
RCTs were associated with greater effect sizes than
RCTs not stopped early. This difference was
independent of the presence of statistical stopping
rules and was greatest in smaller studies.
|
Our results have important implications for
systematic reviews and ethics. If reviewers
do not note truncation and do not consider
early stopping for benefit, meta-analyses
will report overestimates of effects.
...
data monitoring committees ...
have an ethical obligation to future
patients who need to know more than whether
data crossed a significance threshold; these
patients need precise and accurate data on
patient-important outcomes, of both risk and
benefits, to make treatment choices. Such
patients will often number in the tens or
hundreds of thousands and sometimes in the
millions. To the extent that substantial
overestimates of treatment effect are widely
disseminated, patients and clinicians will
be misled when trying to balance benefits,
harms, inconvenience, and cost of a possible
health care intervention. If
the true treatment effect is negligible or
absent—as our results suggest it sometimes
might be—acting on the results of a trial
stopped early will be even more
problematic. Thus, for trial
investigators, our results suggest the
desirability of stopping rules demanding
large numbers of events. For clinicians,
they suggest the
necessity of assuming the likelihood of
appreciable overestimates of effect in
trials stopped early.
|
|
A parallel case:
|
BBC
News
April 8, 2008
Halted drug trial safety concerns
The benefits of some cancer drugs may be exaggerated
as a rising number of trials are stopped early,
experts say.
Italian researchers analysed 25 trials, including
some for the breast cancer therapy Herceptin, that
were stopped early between 1997 and 2007.
The Mario Negri Institute team said data from many of
the recent cases had been used to get drug licences
before the long-term impacts were known.
But drug firms said finishing trials early saved
lives.
The Annals of Oncology report showed that of the 25
trials randomly chosen, 14 had been stopped in the
past three years.
And of these, 11 were used to support applications
for marketing authorisation from regulators.
Lead researcher Dr Giovanni Aplone said the increase
in early conclusions to trials suggested drug firms
were using good interim results to get their products
to market more quickly.
But he warned: "Data on
effectiveness and potential side-effects can be
missed by stopping a trial early."
He admitted there was no hard evidence of this, but
said there was an in-built bias
in the system because trials were often only stopped
early because the results were positive, when
this could just be a "random
high".
Positive results
Meanwhile, those that did not show such positive
results were given more time to prove their worth.
The team found that the
average study duration was 30 months - when the
long-term impact could only be judged over years.
The report also said some trials only enrolled less
than 40% of the total patients planned.
Researchers said regulators needed to take into
account the impact of stopping a trial early when
making decisions about licences.
And they added there needed to
be more use of independent monitoring committees
to verify trial data. Only the largest trials tend to
take this approach.
Professor Stuart Pocock, an expert in medical
statistics from the London School of Hygiene and
Tropical Medicine, agreed the issue was a
problem not just for cancer drugs but all kinds of
treatment.
He acknowledged trial organisers faced a dilemma when
results were positive because those patients involved
in the studies, but not receiving the therapies, could
lose out.
But he added: "We need proof beyond reasonable doubt
to stop a trial early."
...
|
|
All three of the Random Clinical Trials of
circumcision to prevent infection of men, were cut
short early, "because circumcision worked so well". The Ugandan trial of
transmission from HIV+ men to women was cut
short early because it was "futile".
If the African studies had not been stopped early and
long-term results had been obtained, the HIV infection
rate might very well have become statistically
insignificant between the circumcised and
non-circumcised groups. Look at the progression in the
number of cases of HIV in the Kisumu study:
Period since
Start of study |
Circumcised
(n=1391) |
Not circumcised
(n=1393) |
| 0- 1 month |
4 |
1 |
| 1- 3 months |
2 |
3 |
| 3- 6 months |
5 |
9 |
| 6-12 months |
3 |
18 |
| 12-18 months |
0 |
7 |
| 18-24 months |
8 |
9 |
The number of cases in each period for each group is
small, so their relative sizes are affected greatly by
random variation. It appears from the data that the
rate of infection is lower among the circumcised men
in the first 18 months following circumcision, but
that there's little difference beyond 18 months. If
the study had not been terminated early at 24 months,
it is quite likely that the number of HIV cases
between the groups would have become insignificant.
The decision to terminate the studies early prevented
any future comparison of the progression of HIV in the
circumcised and control groups and the very real
possible invalidation of the alleged "proof".
One of the researchers (Gray) has the nerve to
extrapolate the figures into the future from his
truncated study, claiming to show that the rate of
"protection" increases over time:
|
Title:
CROI:
Circumcision
could particularly benefit higher-risk
men
Author: Carter M | Cairns G
Corporate Author: AIDSMAP
Source: 4 Mar 2007
Abstract:
Clinical trials may have understated the
HIV prevention benefit of circumcision,
according to the lead investigator on a
recently reported study. The benefit
appears to grow over time and may be
highest in men with multiple partners, the
Fourteenth Conference on Retroviruses and
Opportunistic Infections heard this week
in Los Angeles. As already reported, two
trials of circumcision as an HIV
prevention measure for men in Rakai,
Uganda and Kisumu, Kenya were halted early
last December when it became apparent that
in both trials circumcision had
approximately halved the risk of acquiring
HIV. Ronald Gray, lead investigator of the
Rakai trial, gave more details to the
Fourteenth Conference on Retroviruses and
Opportunistic Infections in Los Angeles
last week. He said that the benefit of
circumcision was probably greater than the
preliminary efficacy of 51% would
indicate. This is both because the
benefit, for reasons as yet unclear,
appears to grow over time and because the
highest-risk men, namely those with
multiple partners and/or with genital
ulcer disease, appeared to particularly
benefit. Gray told the conference that the
protective effect of circumcision appeared
to increase over time. HIV incidence for
circumcised men was 1.19% a year from 0-6
months after circumcision [14
cases], 0.42% from 6- 12
months [5 cases]
and 0.40% from 12-24 months [3
cases]. This reduction over
time was statistically significant too
(p=0.0014). The corresponding incidence
rates in uncircumcised men for the same
time periods were 1.58% [19
cases], 1.19% [14
cases] and 1.19% [12
cases]. Gray said that
circumcision appeared to protect against
some, but not all, other sexually
transmitted infections.
|
One probability is that the incidence in the first
six months is higher because they got HIV from their
circumcisions! - if there is any non-random causal
relationship at all.
It is utterly innumerate to extrapolate anything from
such tiny numbers of cases, p-values or not. If he'd
done the same to the intact men, he'd find the
"protection" from being intact increased over time
too!
|
A
mathematical extrapolation of that study claims that mass
circumcision "could avert 2.0 (1.1-3.8) million new HIV
infections and 0.3 (0.1-0.5) million deaths over the next ten
years in sub-Saharan Africa. In the ten years after that, it
could avert a further 3.7 (1.9-7.5) million new HIV infections
and 2.7 (1.5-5.3) million deaths."
This has been widely broadcast around the world with new
headlines like "Circumcison could save millions - WHO" (Dominion
Post, Wellington New Zealand, July 12, 2006)) - even though the
new paper is nothing but a mathematical work up of the Auvert
study, which actually found a mere 29 (49-20) circumcised men
who did not contract HIV in 21 months - compared with 20
circumcised men who did contract HIV.
In other words, each of those 29 men has been extrapolated to
more than 125,000 infections and 93,000 deaths prevented - an
outrageous assumption from such a small number.
The paper's authors assume (without saying) that:
- Circumcision is cost-free and risk free
- All circumcisions are equivalent
- Circumcision has no effect on sexual behaviour
- A programme of mass circumcision will have no effect on
other AIDS-prevention programmes
- Men will volunteer for circumcision regardless of the
riskiness of their sexual behaviour.
All these assumptions are false.
This study has been quite invalidated
by the November 2007 announcement that the
number of HIV cases worldwide is much lower than was
previously estimated.
The study's authors are Brian G. Williams, James O.
Lloyd-Smith, Eleanor Gouws, Catherine Hankins, Wayne M. Getz,
John Hargrove, Isabelle de Zoysa, Christopher Dye and Bertran
Auvert. Auvert is the lead researcher of the first of the three
studies (Orange Farm, South Africa) making the claim that
circumcision protects against HIV. According to the paper, he
proposed the development of the model used and was one of those
who developed and applied the model.
Auvert himself did not (at first) advocate circumcision:
|
Medscape
Dr.
Wainberg: Are we ready as a world to make
recommendations in regard to more widespread
surgical procedures such as male circumcision?
Dr.
Auvert: The answer is no. For sure we have a
clear scientific answer about the association
between circumcision and HIV infection. For sure we
have demonstrated that in South Africa and this part
of the world we did see a population level reduction
of HIV infection in this trial, but we are not ready
to use this as a prevention method right now. The
situation in Africa is quite complex -- you've got a
lot of different cultural situations and it's not
possible.
|
|
The
Lancet 2006; 368:1236
DOI:10.1016/S0140-6736(06)69513-5
Correspondence
Cautious optimism for new HIV/AIDS
prevention strategies
Edward
Mills a and Nandi Siegfried b
The
2006 International AIDS Conference, showcased in the
special (Lancet) Red issue, was filled with promises
for effective prevention strategies. Media attention
and plenary speeches suggested that effective
strategies, notably male circumcision and
pre-exposure prophylaxis (PREP), are imminent.1
Instead we advise cautious optimism.
The inferences drawn from
the only completed randomised controlled trial (RCT)
of circumcision could be weak
because the trial stopped early.2
In a systematic review of RCTs stopped early for
benefit,3 such RCTs were found to
overestimate treatment effects. When trials with
events fewer than the median number (n=66) were
compared with those with event numbers above the
median, the odds ratio for a magnitude of effect
greater than the median was 28 (95% CI 11-73). The
circumcision trial recorded 69 events, and is
therefore at risk of serious effect overestimation.
We
therefore advocate an impartial meta-analysis of
individual patients' data from this and other trials
underway before further feasibility studies are
done.
Although the rationale for PREP is
exciting, researchers have leapt from small
(n=6-18) and inconsistent non-randomised monkey
studies into multicentred trials.4 The
first PREP trial results were provided at the
conference,5 but had an insufficient
number of infections to provide any inferences
about effectiveness (two of 363 vs six of 368).
New
interventions are required to slow the HIV/AIDS
pandemic. Disappointments stemming from media hype
and misinterpretation of early trials can make
policy and recruitment of appropriate trial
populations difficult. If we are to alter the
epidemic's progress, we should be methodologically
rigorous, and cautiously optimistic about the
potential for new interventions.
We
declare that we have no conflict of interest.
References
1.
Saletan W. When cutting isn't cruel. Washington Post
Aug 20 2006; B02.
2.
Siegfried N. Does male circumcision prevent HIV
infection?. PLoS Med 2005; 2: e393. CrossRef
3.
Montori VM, Devereaux PJ, Adhikari NK, et al.
Randomized trials stopped early for benefit: a
systematic review. JAMA 2005; 294: 2203- 2209.
CrossRef
4.
Mills EJ, Singh S, Singh JA, Orbinski JJ, Warren M,
Upshur RE. Designing research in vulnerable
populations: lessons from HIV prevention trials that
stopped early. BMJ 2005; 331: 1403-1406. CrossRef
5.
Peterson L, Taylor D, Clarke EEK, et al. Findings
from a double- blind, randomized, placebo-controlled
trial of tenofovir disoproxil fumarate (TDF) for
prevention of HIV infection in women. XVI
International AIDS Conference; Toronto, Canada; Aug
17, 2006. Back to top
Affiliations
a.
Centre for International Health and Human Rights
Studies, 1255 Sheppard Avenue East, Toronto, Ontario
M2K 1E2, Canada
b.
Clinical Trial Service Unit, Department of Medicine,
University of Oxford, Oxford, UK
|
|
The Hawthorne Effect
The
Hawthorne
effect refers to the phenomenon that when people
are observed in a study, their behavior or performance
temporarily changes. Others have broadened the
definition to mean that people’s behavior and
performance change, following any new or increased
attention. The term gets its name from a factory
called the Hawthorne Works in Illinois, where a series
of experiments on factory workers were carried out
between 1924 and 1932. Most notably, production went up
when the lighting was increased, and it went up
when the lighting was decreased: it was the
attention the workers were getting when the
measurements were taken, not the lighting, that caused
the effect.
The Randomised Controlled Trials are subject to the
Hawthorne Effect because they were not double blind:
all the subjects knew which group they were in, and
what effect this was supposed to have. The Hawhtorne
Effect could not have directly affected the extent to
which they were infected with HIV, but it could have
affected their sexual behaviour, making the
circumcised men more aware of safer sexual practises
(having part cut off one's penis concentrates the mind
wonderfully), and perhaps more likely to implement
them. They reported no change in their sexual
behaviour, but self-reporting may not be accurate:
their reporting of homosexual behaviour, for example,
is so low it attracts the strong suspicion that they
were under-reporting it.
|
A comprehensive critique:
Male
Circumcision and HIV Prevention:
Is There Really Enough of the Right Kind of
Evidence?
Gary
W Dowsett, Murray Couch
"At Toronto, sociologists and anthropologists in
particular were sceptical of the narrow form of
''science'' being touted as the only form of evidence
needed. Activists and practitioners, e.g. people
living with HIV and AIDS, those working in the
non-governmental sector and prevention workers - those
who comprise the bulk of the ''AIDS community'' - were
concerned with a potential undercutting of their
hard-won shifts in sexual cultures, in many places,
toward safe sex practices." ...
"After all, these trials were not test tube
experiments but experiments conducted in clinical
settings. Such settings are profoundly social moments
with real human interactions and complex components,
even if RCT design in principle tries to circumvent
such inputs. For example, how
do we assess the fact of these trials not being
double-blinded: the men in each arm clearly knew
their circumcision status? That known difference
could have affected how the men responded
behaviourally, psychologically and sexually."
A literature search found a much greater proportion
of the studies of circumcision were of adverse
effects, ethics, ethnology, history, legislation and
jurisprudence, than (the proportion) of the studies of
appendectomy ("the surgical removal of a part of the
body seen as somewhat unimportant") or hysterectomy
("a more serious and controversial sexual and
reproductive health operation") .
From the conclusion:
"We believe we need to know much more about male
circumcision for HIV prevention before adopting it as
a population health measure. The WHO/UNAIDS Statement
is cautious in noting the existence of caveats and
gaps, but it argues that it is time to go ahead. We
would argue that there is still much work to do before
national authorities and the global HIV/AIDS community
can feel confident about proceeding."
Reproductive Health Matters
2007;15(29):33-44
|
Gary Dowsett was the only person the least
bit skeptical about the benefits of genital cutting who was
invited to the WHO/UNAIDS meeting at Montreux, Switzerland in
2007 where genital cutting was set as a mass intervention to
protect against HIV. As Intactivists suspected, the meeting was
gerrymandered by circumcision advocates Daniel Halperin, Robert
Bailey, Robert Gray and others to rubberstamp their
recommendation.
How the WHO was manipulated into
promoting genital cutting as
an HIV prevention
|
Global Public Health,
Hybrid forum or network?
The social and political construction of an
international ‘technical consultation’:
Male circumcision and HIV prevention
Alain Giami, Christophe Perrey, André Luiz de
Oliveira Mendonça & Kenneth Rochel de Camargo
Abstract
The technical consultation in Montreux, organised by
World Health Organization and UNAIDS in 2007,
recommended male circumcision as a method for
preventing HIV transmission. This consultation came
out of a long process of releasing reports and holding
international and regional conferences, a process
steered by an informal network. This network's
relations with other parties is analysed along with
its way of working and the exchanges during the
technical consultation that led up to the formal
adoption of a recommendation. Conducted in relation to
the concepts of a ‘hybrid forum’ and ‘network’, this
article shows that the decision was based on the
formation and consolidation of a network of persons.
They were active in all phases of this process,
ranging from studies of the recommendation's efficacy,
feasibility and acceptability to its adoption and
implementation. In this sense, this consultation
cannot be described as the constitution of a ‘hybrid
forum’, which is characterised by its openness to a
debate as well as a plurality of issues formulated by
the actors and of resources used by them. On the
contrary, little room was allowed for contradictory
discussions, as if the decision had already been made
before the Montreux consultation.
Excerpts:
There was but one avowed opponent in this group: Gary
Dowsett, an Australian sociologist who had extensive
experience in social science research on AIDS and had
served as consultant for WHO and other international
organisations. As one of a group of self-identified
gay researchers, his activities in this field reached
back to the mid-1980s. Nonetheless, the possibility
for him to present his critique was limited by both
the agenda and the perceived hostility towards him
during discussions by, in particular, a major US
epidemiologist, one of the recommendation’s principal
advocates. During our interview, Dowsett cited this
person’s name, which we have replaced with the pronoun
HE in the transcripts:
I’m standing in the hotel, with a glass of
champagne and HE … comes charging over to me,
immediately … and just started to attack me,
immediately, and … ‘How wrong I was! Why I was doing
this? I got the argument wrong – Did I not understand
how important all this was’ … and HE attacked me …
every time I spoke in the meeting at Montreux. Every
time!
...
According to some interviewees, the time devoted to
the presentations did not allow for a genuine, open
debate, in particular about how to extrapolate from
the findings in the narrow context of the RCTs to the
general population. This question was thought to be
settled, given the results from previous observational
and epidemiological studies. There was no mention of
the contradictory findings that had been published,
nor of a scientific controversy. According to Dowsett
during our interview, Hankins’ speech on the second
day barely mentioned the recommendation’s social and
cultural consequences:
We were concerned about the cultural consequences
of circumcision in terms of shifting ideas of
sexuality, sexual cultures and masculinity; and any
evaluation of circumcision being rolled out needed to
include much broader social and cultural markers than
simply medical and behavioural markers of the
implementation. That was part of the recommendations
for the research agenda, from the social science
meeting in Durban. That was simply reported in
Montreux, and nothing was either endorsed or done
about it. It was just presented as background
information.
|
Followup in South Africa: Correlation is not causation
|
Circumcision
October 3, 2013
Aidsmap
Cross-sectional study suggests circumcision is having
a big impact on HIV rates among men in Orange Farm,
South Africa
by Michael Carter
Research conducted in South Africa suggests that the
roll-out of circumcision is reducing the prevalence and
incidence of HIV among men. Published in PLOS
Medicine, the study also showed circumcision does
not lead to the adoption of riskier sexual behaviour
that could potentially cancel its benefits.
The French researchers who conducted the study [the
very
same people who made the original claim]
believe its findings support the accelerated roll-out of
circumcision programmes for men living in settings with
high HIV prevalence.
The results of three randomised controlled trials
published between 2005 and 2007 showed that circumcision
reduced men’s risk of infection with HIV by between 50
and 60%. As a result, since 2007 both UNAIDS and WHO
have recommended that voluntary medical male
circumcision (VMMC) programmes should be incorporated
into prevention initiatives in settings with a high HIV
prevalence.
However, little is known about the impact of
circumcision roll-out programmes on the spread of HIV
among men. [And isn't that a
scandal in itself?]
French investigators from the Bophelo Pele project
designed a cross-sectional study involving men in the
Orange Farm township in South Africa. The first
randomised controlled trial to test the effectiveness of
VMMC on HIV acquisition was conducted in the township
between 2002 and 2005.
Roll-out of VMMC started in Orange Farm in 2008 and
between 2007 and 2008 the French investigators recruited
1998 men between the ages of 15 and 49 years to a
baseline survey. The men were tested for HIV, their
circumcision status was determined and demographic data
were collected. The men were also asked about their
sexual risk behaviour, including condom use and number
of non-spousal partners.
A follow-up survey was conducted in 2010 and 2011 and
involved 3388 men. [So at
least 1/3 of the men were not in the first part of
the "follow-up" study". Strange.]
The investigators calculated the prevalence of
circumcision, compared HIV prevalence rates and sexual
risk behaviour between circumcised and uncircumcised men
and calculated the impact of circumcision roll-out on
HIV incidence.
Circumcision prevalence increased from 17% in the
baseline survey to 53% in the 2010-2011 survey.
“This study has shown that the roll-out of free VMMC
can lead to a substantial uptake in just a few years,”
comment the authors.
There were no significant differences in the [reported]
sexual behaviour of circumcised and uncircumcised men.
The proportion of circumcised and uncircumcised men
reporting consistent condom use in the previous twelve
months was 44 vs 45%. The proportion reporting two or
more non-spousal partners was 50 vs 44%.
The HIV prevalence rate among uncircumcised men was 19%
compared to 7% among circumcised men with an overall
prevalence rate of 12%. [But
we know that in 10 out of 18 other countries for
which USAID has figures, the ratio is the other way.
This could be unconnected to circumcision.]
The investigators calculated that it would have been
15%, almost a fifth higher, if the circumcision
programme had not been rolled out.
[Assuming what they want to prove, that genital
cutting is efficatious against HIV.]
Moreover, the authors also calculated that the roll-out
of VMMC reduced the incidence of new HIV infections by
between 57 and 61%.
“The roll-out of VMMC in this community was associated
with a reduction in the prevalence and incidence of HIV
among circumcised men in comparison with uncircumcised
men, and we estimate that without this project, HIV
prevalence averaged on all adult men would have been
significantly higher,” write the authors.
They acknowledge that their study has limitations,
chief among these its cross-sectional design. As
the study was not randomised, it could not prove a
causal relationship between circumcision status and
the risk of HIV infection.
Nevertheless, the authors believe their research shows
the value of circumcision and conclude: “the main
implication of this study is that the current roll-out
of adult VMMC…should be accelerated.” [And
Carthage
must be destroyed.]
|
Followup in Uganda: Is there even correlation?
|
Aidsmap
February 27, 2015
Circumcision is reducing HIV incidence in Uganda,
Rakai community study shows
by Keith Alcorn
The growing uptake of medical male circumcision by men
in the Rakai district of Uganda is leading to a
substantial reduction in HIV incidence among men in one
of the districts of the country worst affected by HIV,
Xiangrong Kong of Johns Hopkins Bloomberg School of
Public Health told the Conference
on
Retroviruses and Opportunistic Infections (CROI 2015)
in Seattle, USA, on Thursday.
Three large clinical trials in sub-Saharan Africa,
including one conducted in the Rakai district [by
the authors of this follow-up study],
have shown that medical male circumcision reduces the
risk of acquiring HIV by between 50% and 60%. These
findings have led to the scale up of services offering
medical circumcision to men, especially to adolescents
and young men.
However, until now, the only evidence of an impact of
medical male circumcision on HIV incidence in the
communities where it is offered has come from a
cross-sectional study in the Orange Farm community in
South Africa, where another of the clinical trials
showing efficacy took place. That
study
showed that the roll out of circumcision had reduced
HIV incidence by between 57% and 61%.
The study conducted in Rakai set out to assess the
impact of scaling up circumcision in Rakai district
since 2007, through analysis of annual cross-sectional
surveys of adults aged 15-49 carried out by the Rakai
Community Cohort Study. The analysis excluded Muslim men
who would have been circumcised in any case [did
they have an embarrassingly high HIV rate?],
and sought to assess the impact of circumcision as an
HIV prevention intervention. The analysis also assessed
and controlled for the level of antiretroviral coverage
over time in women, since increased antiretroviral
coverage would be expected to reduce HIV transmission to
men, regardless of the level of circumcision.
The study found that circumcision coverage in
non-Muslim men increased from 9% during the Rakai
circumcision study to 26% by 2011, four years after the
trial concluded. Every 10% increase in circumcision
coverage was associated with a 12% reduction in HIV
incidence (0.88, 95% confidence interval 0.80-0.96). [Was this only among the
circumcised men, or also among the intact? In other
words, did the circumcision campaign just raise
public awareness of HIV prevention, and promote
safer practice overall?]
However, there was no evidence of a reduction of
incidence in women as a consequence of the reduction in
HIV prevalence in men due to circumcision. [A
study by these same authors started to find an increase
in the incidence in women, but they ignore this
possibility.] Dr Xiangrong Kong said that
previous modelling studies suggested it may take up to a
decade for medical male circumcision to have an impact
on HIV incidence in women. [Why
so long?]
Preliminary data for 2013-14 show that the proportion
of non-Muslim men who have undergone medical
circumcision in the Rakai Community Cohort has increased
to 49%.
|
A damning critique of the ethics of
these experiments
|
Developing
World Bioethics, Wiley Online Library, 09
September 2020 https://doi.org/10.1111/dewb.12285
A new Tuskegee? Unethical human
experimentation and Western neocolonialism in the
mass circumcision of African men
Max Fish, Arianne Shahvisi, Tatenda Gwaambuka,
Godfrey B. Tangwa, Daniel Ncayiyana, Brian D. Earp
Abstract
Campaigns to circumcise millions of boys and men to
reduce HIV transmission are being conducted throughout
eastern and southern Africa, recommended by the World
Health Organization and implemented by the United
States government and Western NGOs. In the United
States, proposals to mass?circumcise African and
African American men are longstanding, and have
historically relied on racist beliefs and stereotypes.
The present campaigns were started in haste, without
adequate contextual research, and the manner in which
they have been carried out implies troubling
assumptions about culture, health, and sexuality in
Africa, as well as a failure to properly consider the
economic determinants of HIV prevalence. This critical
appraisal examines the history and politics of these
circumcision campaigns while highlighting the
relevance of race and colonialism. It argues that the
“circumcision solution” to African HIV epidemics has
more to do with cultural imperialism than with sound
health policy, and concludes that African communities
need a means of robust representation within the
regime.
|
|
|